A quick look at CMS cut point announcements and the impacts of triple-weighted quality measures becomes clear. Medicare Advantage plans need optimized adherence strategies to see rewards in the Star Ratings program. Success requires plans to make the most of medications, and that means understanding the intricate nature of their member population’s behaviors.
The Data on Adherence Barriers
We’re seeing a growing body of research (which mirrors our own) showing just how much cost impacts medication adherence. In the last year, one survey in particular has drawn significant attention to the issue. The survey reported that, out of the 63% of respondents who received a prescription in the last three months:
- 97% filled it
- 67% (of those that did not fill) did not fill because costs were too high
- 25% missed at least one dose after filling
It’s also important to note that 29% of respondents quit taking their medication without telling their provider. Interestingly, cost was not the primary reason for this. In fact, these respondents quit taking the drugs because:
- They experienced unwanted side effects (29%)
- They “didn’t need it anymore” (17%)
- They “felt better” (16%)
- The medication “wasn’t working” (15%)
- The drugs were priced too high (10%)
This tells us that, overall, members are concerned about costs prior to filling prescriptions, but then become non-adherent after filling them for a variety of other, often subjective, reasons.
Member Adherence Behavior Data – Collection and Application
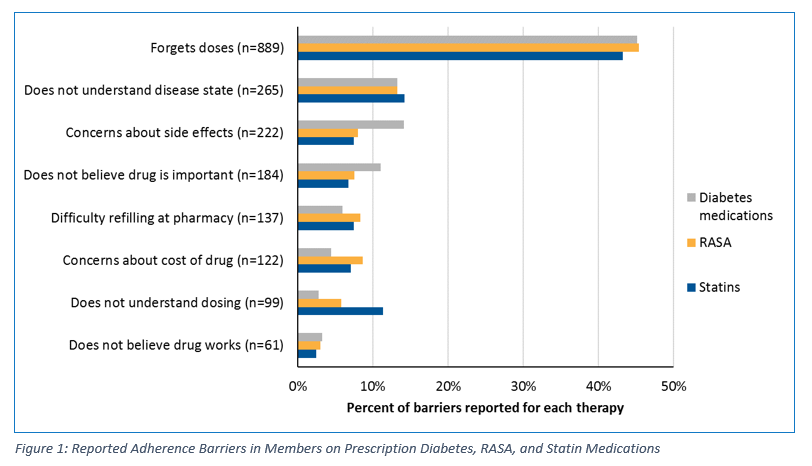
In collaboration with our clients, member data is gathered and used to inform clients’ quality measure performance strategies. High-level barrier reporting data aligns with the previously mentioned survey’s data for members who quit taking medications. (See Fig. 1 for an excerpt of findings from a regional health plan client.) Primary barriers to medication adherence in this data include forgetfulness, understanding of their own physical condition or the drug, transportation/ease of filling at the pharmacy, and cost.
The Role of Member Behavior in Medication Adherence
Understanding and establishing relationships with members is necessary to driving real adherence change. To that end, we use intervention calls to talk to the member, educate them if they need it, and record data on why they’ve missed doses or abandoned prescriptions altogether. Our pharmacy service representatives and pharmacists have deep conversations with members to help identify root non-adherence causes. This allows us to develop sustainable, scalable resolutions that help plans use behavior modification by:
- Informing better-targeted, more personal interventions (e.g., RxEffect can house barrier reporting, fill dates, notes from previous intervention attempts, and more).
- Helping aggregate these insights and apply them to adherence strategies
- Promoting approaches that help members overcome barriers.
- Adjusting intervention tactics to those that achieve the most positive outcome (e.g., facilitating warm transfers to the pharmacy or involving member’s prescribers/providers).
Beyond Behaviors – Achieving Quality Measure Success
Improving medication adherence requires data analysis and prediction, but it’s more than that. Plans must be able to tap into the ways in which their own member’s behaviors impact their adherence. It won’t be the same from population to population or plan to plan, so implementing tailored, data-based strategies to create valuable interventions will be critical to success. This will be the way forward to not only improve adherence, but also enhance member satisfaction and health.
We have been doing this for clients for years – refining cut-point strategies, workflow and network solutions, and analytic methods to drive substantive change among member populations. However, we understand many Medicare Advantage plans simply don’t have the time or resources to do the same. Let our experience and expertise work for you – let’s talk about what you need.