Restricted Content
Please fill out the form below to access this content.
By 2035, seniors (those aged 65 years or older) will outnumber children (those aged 18 years and younger).1 At that time, every baby boomer in the U.S. will be “retirement age” — and therefore Medicare age. That translates to approximately 78 million seniors, or one in every five residents, accessing healthcare under the Medicare umbrella.
“At a time when older patients have the greatest need to communicate with their physicians, life and physiologic changes make it the most difficult.”2
Understandably, the healthcare industry has paid quite a bit of attention to these statistics. Experts have considered everything from how health evolves across generations to what trends we can expect as baby boomers enter Medicare and beyond.3, 4, 5, 6 As risk-bearing entities associated with these populations, Medicare Advantage health plans are seeking sustainable solutions to prepare for and support this growing member population. Examining the research, news, and activities involving the Medicare population reveals three trends: chronic conditions, quality care, and dual Medicare/Medicaid eligibility. Plans seeking to thrive will need to focus their ongoing efforts on the impacts medication adherence, cost containment and quality improvement, and dual-eligible programs have on seniors.
WHAT’S BEING STUDIED: CHRONIC CONDITIONS
“Chronic diseases and conditions—such as heart disease, stroke, cancer, [T]ype 2 diabetes, obesity, and arthritis—are among the most common, costly, and preventable of all health problems.”7
It should come as no surprise that some of the most researched aspects of healthcare relate to chronic conditions such as heart disease and diabetes. Despite a wide array of drugs that exist to treat and manage these conditions, they remain among the leading causes of death in the nation.
Additionally, these conditions aren’t new players in the healthcare space, especially for seniors. What is new, however, is the eye toward the commonalities among the conditions being studied — specifically, the way in which seniors take, think about, and adhere to medications for their condition.
HEART DISEASE
In 2017, the American Heart Association (AHA) released a study showing that Medicare beneficiaries with heart disease who regularly took their medications as prescribed had “less than half the risk of having a cardiovascular event.”10 In actuality, it has been clear for some time that the effectiveness of medication for heart disease requires adherence to those medications.11, 12, 13 The AHA still uncovered some new findings:
- An 80 percent and above adherence rate was found to substantially reduce the odds of patients having cardiovascular events as they age.
- Medicare beneficiaries who are newly diagnosed with heart disease are highly non-adherent to their cardiovascular medications and therefore more likely to have cardiovascular episodes and incur higher medical costs as a result.
Also of some note was that the AHA study was able to conclude “long-term adherence is more strongly associated with [negative] cardiovascular outcomes compared with first year adherence among older beneficiaries.”
“An analysis of adherence to medications used to treat diabetes, dyslipidemia, and hypertension estimated that the direct cost of poor adherence was $105.8 billion in 2010 across 230 million patients, which represented $453 per adult.”14
DIABETES
The exact numbers related to diabetes and medication adherence are often contested in the field, given the variable ways in which adherence has been measured.15 The need for medication adherence among diabetics, however, is never up for debate. Regardless of the numbers used to analyze it, medication non-adherence is one of the major factors preventing those with diabetes from achieving control of their condition and overall health. Furthermore, seniors who are less than 80 percent adherent to diabetes medications cost health plans an average of $5,170 per year.14
MEDICAL COST SAVINGS AND MEDICATION ADHERENCE RATES
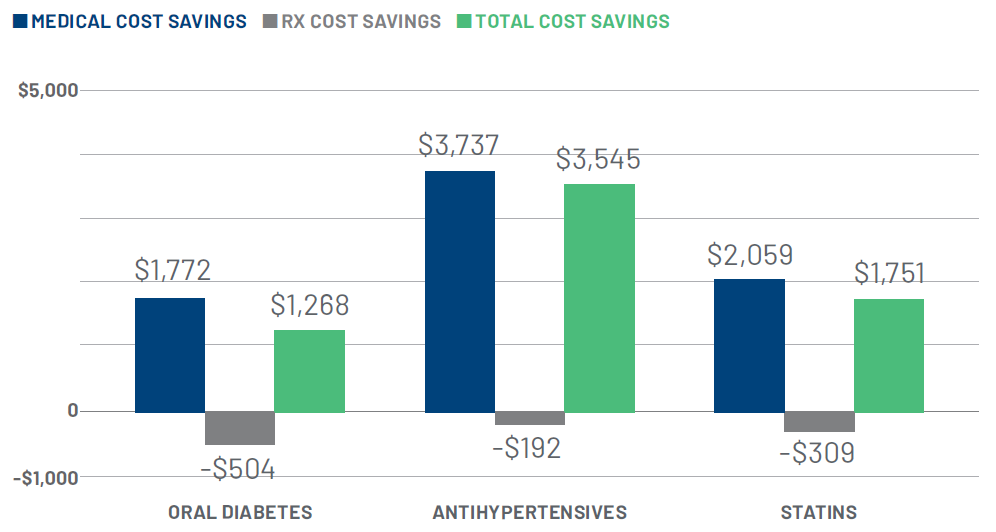
The data around chronic conditions and medication adherence align closely with RxAnte’s own research. Specifically, there is a clear relationship between medical cost savings and adherence among members. For example, when analyzing the Medicare population of a large regional health plan client, we found that members who adhered to prescribed cardiovascular therapies are .89-2.76 percent less likely to undergo cardiovascular procedures (see Fig. 1). Similarly, when members are adherent to prescribed diabetes and cardiovascular treatments, plans can net thousands of dollars in annual, per member savings (see Fig. 2).
Figure 1: Cardiovascular procedure rates are lower among members adherent to drug therapies
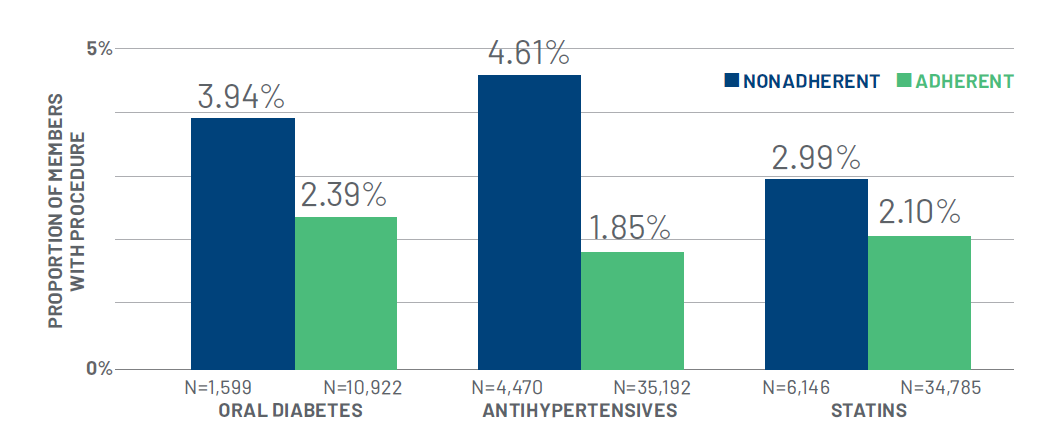
Figure 2: $1,200-$3,500 medical cost savings among adherent members with diabetes or cardiovascular conditions
PERSISTENT MEASUREMENT, CONTINUOUS EVOLUTION
Chronic diseases and conditions are being studied in the U.S. with more intensity and interest than ever before for several reasons, not the least of which is the rapidly growing Medicare population. Understanding which conditions seniors are at the highest risk for and how to manage those conditions is a critical foothold for healthcare leaders to gain sooner rather than later. This will require persistent attention to the population as they age and continually evolving methods that work to keep seniors healthy.
RXANTE INSIGHT
CEO JOSH BENNER ON EVOLVING COMMUNICATIONS WITH SENIORS
“Seniors can be a particularly difficult population to access via technology. Although updated technology and software are incredibly useful in healthcare for obvious reasons, technology as a communication tool can actually have negative effects on seniors. The key is not to ask this generation to adapt to technology, but to use the technology to amplify and improve our approach to communicating with them.
We do this by using our platform to examine patient data (demographic, geographic, physical, etc.), and identify which patients need intervention and the best time and way to reach them. For seniors specifically, most don’t want to receive a text asking them if they’re taking their medications, they want to speak with a human being. They don’t want to search the internet for side effects or interactions, they want to ask a live person. That’s where our call centers come in.
The call center employees reach out to the senior patients to determine why they may not be adhering to their medications. Based on the patient’s reasoning, the employees can connect them with proper resources (their physician, health plan, etc.).
Using our technology to measure and evolve, enables rather than replaces human interaction, and that produces improved outcomes and satisfaction among senior members.”
WHAT’S BEING SAID: COSTS AND QUALITY
“While some plans have experienced administrative and operational challenges in implementing outcomes-based contracts, most are figuring out ways to benefit from these types of contracts in multiple therapeutic areas… Solutions in data connectivity, contract monitoring, and direct clinician intervention streamline the administrative burden and enable transparency for all parties.”16
A quick internet search for news related to “healthcare” will yield over 800 million results. Out of the top ten, six are specifically related to healthcare costs. A search for news related to “Medicare” will produce only eight million results. For “Medicare Advantage Plans”, the number is 80,000. All maintain a similar trend of cost-related articles. At first glance, it can be easy to mistake this as an indicator that cost is the focus of the conversation. However, although costs are certainly a symptom, they aren’t the entire problem. Another common thread in the dialogue is the rising demand for better quality care.
For better or worse, the entire conversation can be summed up with the old adage “you get what you pay for.” As health plans strive to meet the need for quality care among the Medicare population or otherwise, they will also have to lower costs. They will need to make better use of technologies, employing data-powered systems that tackle the root problems members have. To start with, plans will need to examine ways to integrate treatments and medical management and to use clinician interventions to improve medication adherence. Without a high-level shift in the industry, this simply isn’t achievable. Enter the transformation of healthcare payment models from “fee-for-service” to “value-based.”
“Health care economists estimate that 40–50 percent of annual cost increases can be traced to new technologies or the intensified use of old ones.”17
VALUE-BASED CARE
Not long ago, Centers for Medicare & Medicaid (CMS) expanded the definition of “primarily health-related” care and added new supplemental benefits. These are tremendously impactful to the Medicare population.18 Specifically, they offer seniors the following:
- Improved prescription drug prices via increased competition and relaxed rules around generics.
- New services and coverage to include those that “increase health and improve quality of life,” such as non-skilled in-home care and assistance devices.
- Updates to the “Patients Over Paperwork” initiative that “works to remove regulatory obstacles and empower patients to make informed healthcare decisions; develop innovative approaches to improving quality, accessibility, and affordability; and improve beneficiaries’ customer experience.”19
MEASURING VALUE AND QUALITY
The MedPAC 2018 Report to the Congress made a firm recommendation to “link payment to the quality of care to reward accountable entities and providers for offering high-quality care to beneficiaries.”20 In fact, quite a bit of the report focused on reinforcing care quality by rewarding positive patient experiences, improved outcomes, and increased safety measures. These incentives are tied to plans in a big way, including assessing them “largely on clinical quality or outcome measures such as readmission rates, medication adherence for diabetes medications, and nursing home use.” Plans that are able to effectively reach seniors to improve on these measured areas will be able to reap the rewards in a big way. Even so, it’s important to keep the end goal in mind – quality care for members. Building effective networks and plans will lead to a decrease in costs to patients, too, as care facilities are able to achieve financial success and stability under the new model.
RXANTE INSIGHT
CEO JOSH BENNER ON HEALTHCARE QUALITY
“I am particularly excited about accountability in healthcare. With value-based care, we’re now paying for value instead of efforts and services. This is changing everything. We [the healthcare industry] have started thinking about what value is and what is the value we want to pay for. We have to think about the outcome we want to create if we’re going to pay providers accordingly. This is increasing providers’ responsibility.
There’s also now accountability for how medications are prescribed and taken. This accountability is rapidly transferring from government payers to commercial payers to providers and pharmaceutical companies. Imagine what would happen if the accountability transferred to the patients – what if we started paying patients to take their medications? I think there are a lot more changes to come when it comes to accountability and healthcare.”
“Aspects of the MA program that help health plans optimize revenue (e.g., quality bonuses and risk adjustment) are important drivers of VBC strategy in MA. Medicare Star Ratings bonuses and other quality-focused initiatives encourage a systematic approach to quality improvement that is best achieved through health plan and provider collaboration.”21
QUALITY AND MA PLANS
CMS may have taken the reigns in the last decade on value-based care, but in 2015 health plans were still expecting CMS to do more.21 Plans hoped CMS would improve its methods of boosting adoption to the new model. They have also been known to be concerned about the impact decreasing inpatient admissions would have on their revenue.
More recently, health plans are relieved to see data that reveals post-acute care rather than inpatient admissions, is where this model’s impact comes from.16
THE COST OF QUALITY
Healthcare models have traditionally been fee-for-service. It’s only been in the last decade that legislation like the Affordable Care Act started tipping the scales in favor of value-based care. Although both the healthcare industry and patients alike are ready to see increased value at lower costs, the simple truth is that the foundation is still being laid. Healthcare organizations will have to take the lead on improving in areas that impact patient outcomes. Plans will need to build quality by enforcing methods that impact patient engagement, provider empowerment, and medication adherence — especially for seniors.
WHAT’S BEING DONE: DUAL-ELIGIBLE DEMONSTRATION PROGRAMS
“Individuals who receive both Medicare and Medicaid (known as dual-eligible beneficiaries) often have complex health needs but are at risk of receiving fragmented or low-quality care because of the challenges in obtaining care from two distinct programs.”20
CMS has been working on providing dual-eligible beneficiaries with better service for many years. The intent has been to bring these high-risk individuals into a plan that offers:22
- Improved and simplified access to benefits of Medicare and Medicaid
- Better quality short and long-term care
- Clearer explanations and education of plan coverage
- Increased care coordination and transitions
To bring that vision to life, Medicare offers four plans: the demonstrations Medicare- Medicaid Plans, Medicare Advantage dual-eligible special needs plans (D–SNPs), fully integrated dual-eligible SNPs (FIDE SNPs), and the Program of All-Inclusive Care for the Elderly. States that have implemented and continued dual-eligible demonstration programs such as these have shown promise. Early analysis indicates the integrated plans can:23
- Improve member experience, especially related to care coordination.
- Have decreased inpatient admissions.
- See net savings of around three percent.
- Create administrative enhancements which can be useful in other programs as well.
RXANTE INSIGHT
CEO JOSH BENNER ON DUAL-ELIGIBLE BENEFICIARIES
“I have three pieces of advice that I always share with entrepreneurs:
- Study the problem that you want to solve and understand it deeply.
- Design a solution that is creative and bold.
- Be relentless in proving and improving the value of the design or solution that you create.
We need to apply these concepts to our approach to dual-eligibles as well. We have done significant digging into the problem of dual-eligibility and integration of Medicare and Medicaid. We continue to dig. We continue to learn new things about them as a population and what that population is going to look like as it balloons with the influx of aging baby boomers.
We have designed a solution (or four!) and they have been bold in their very nature of being new, changing the norm.
Finally, we are in the next phase — relentlessly trying to prove and improve. In spite of difficulties with gathering data, and in spite of the challenge of garnering support and participation — we persist as a nation. And RxAnte persists, too. We have developed and refined and continue to refine our methods of improving medication adherence, a driving factor in improving Medicare and Medicaid outcomes. This is a fight worth fighting.”
KEY AREAS OF ASSESSMENT
The dual-eligible demonstration programs are assessed on four key areas: access to care, service use, quality of care, and cost.20
For seniors, access to care and service use go hand-in-hand. By engaging dual-eligible seniors with their primary care providers more frequently, it is posited that members will be able to avoid costly use of services such as inpatient and post-acute care. These beneficiaries are also encouraged to make use of community-based care that can implement greater levels of preventive care. There is a large body of research showing that preventive care, such as vaccinations, screenings, and lifestyle changes can have positive impacts specifically for seniors.24 Implementing preventive practices via dual-eligible programs could therefore, potentially lead to greater life expectancy, reduced unnecessary utilizations, and decreased readmission rates.
Assessing quality of care among dual-eligible beneficiaries is perhaps the most involved area of evaluation. As we mentioned previously, healthcare organizations are still in the midst of pioneering and understanding how to measure value-based care. However, there are a few well-established quality care measures in the demonstration programs. These include patient experience measures, such as the Consumer Assessment of Healthcare Providers (CAHPs), and clinical quality measures, such as the Healthcare Effectiveness Data and Information Set (HEDIS).
Even examining the program costs will not be easy. The evaluations for all programs are not likely to be available any time soon, with only one annual evaluation having actually been completed to date. The data is difficult to gather, and there have been multiple delays to both quantitative and qualitative analyses. It will take time and greater participation before dual-eligible demonstration programs can show reliable results.
DUAL-ELIGIBLE BENEFICIARIES VS. OTHER MAPD GROUPS
There are many differences in the dual-eligible portion of the senior population. They “are more likely to have functional impairments, behavioral health conditions, and substance abuse disorders.”20 This makes them a costlier group to both Medicare and Medicaid.
Further complicating the program, a disproportionate number of dual-eligible beneficiaries are minorities. This creates both real and possible language and cultural barriers that are not as prevalent in the primary Medicare population.25 Those we are dual-eligible are also categorically the sickest subset of the senior generation. Those in institutions rack up about four times the amount of spending as their counterparts in community care facilities.
TARGETING MEDICARE AND MEDICAID POPULATIONS – SIMULTANEOUSLY
As the group of dual-eligible beneficiaries grows, MAPD plans will need to take on the difficult but rewarding task of targeting both groups. Although they will face the same challenges as CMS does in measuring and creating effective programs, plans need to prepare. MedPAC has recommended policy changes to support plan integration: limiting the allowed frequency with which plans can be changed; limit some enrollment to full-benefit dual-eligible beneficiaries; and increase passive enrollment.20
To prepare for these policies, plans need health technology partners. These partners must be able to implement systems and platforms that are able to measure and provide actionable insights on both populations. For example, RxAnte uses a proprietary algorithm to review the medical/pharmacy claims data of our clients’ members. Outputs of this analysis include prioritized member lists based on urgency, risk, and receptivity to intervention. The analysis also allows us to create detailed recommendations and intervention simulations that optimize population adherence lift.
SENIORS OF TODAY, TOMORROW, AND BEYOND
The real challenges of caring for the elderly in 2030 will involve: (1) making sure society develops payment and insurance systems for long-term care that work better than existing ones, (2) taking advantage of advances in medicine and behavioral health to keep the elderly as healthy and active as possible, (3) changing the way society organizes community services so that care is more accessible, and (4) altering the cultural view of aging to make sure all ages are integrated into the fabric of community life.26
America’s seniors are a unique population. They have lived in times when no one knew that smoking cigarettes caused cancer.27 Now they live in times when your risk of certain cancers can be determined by examining your DNA.28 In another ten to 20 years they will likely live in times where healthcare has become unrecognizable compared to where we are today. They may even live in times where the power of medication exceeds our most hopeful expectations, where perhaps prescriptions can not only control chronic conditions, but can cure them entirely.
In the meantime, seniors (many of them dual-eligible) will be the ones informing chronic disease management, determining the relationship between cost and quality of care. Baby boomers are the first generation to test the efficacy of drugs used to treat long-term and age-related conditions. They will be the voice that determines patient and member satisfaction, setting the stage for the future of outcomes-based care. Those who are dual-eligible will have experiences and outcomes that will change the fate of integrated plans.
Together, today’s seniors and health plans who adapt to their needs, will bring about the realization of lower-cost, higher-quality healthcare.
Resources
- (1)https://www.census.gov/newsroom/press-releases/2018/cb18-41-population-projections.html
- (2)https://www.aafp.org/fpm/2006/0900/p73.html
- (3)https://academic.oup.com/psychsocgerontology/article/64B/3/369/575803
- (4)https://link.springer.com/article/10.1353%2Fdem.2004.0022
- (5)https://www.healthaffairs.org/doi/10.1377/hlthaff.26.5.1417
- (6)https://academic.oup.com/psychsocgerontology/article/55/5/S298/536405
- (7)https://www.cdc.gov/chronicdisease/overview/index.htm
- (8)https://www.cdc.gov/nchs/fastats/deaths.htm
- (9)https://www.cdc.gov/injury/images/lc-charts/leading_causes_of_death_age_group_2016_1056w814h.gif
- (10)http://jaha.ahajournals.org/content/6/6/e006056
- (11)http://circ.ahajournals.org/content/circulationaha/119/23/3028.full.pdf
- (12)https://jamanetwork.com/journals/jamainternalmedicine/article-abstract/623804
- (13)https://www.nejm.org/doi/pdf/10.1056/NEJM198010303031804
- (14)https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4966497/
- (15)https://onlinelibrary.wiley.com/doi/pdf/10.1111/1753-0407.12306
- (16)http://avalere.com/expertise/life-sciences/insights/health-plans-are-actively-exploring-outcomesbased-contracts
- (17)https://www.thehastingscenter.org/briefingbook/health-care-costs-and-medical-technology/
- (18)https://www.cms.gov/Newsroom/MediaReleaseDatabase/Press-releases/2018-Press-releasesitems/2018-04-02.html
- (19)https://www.ajmc.com/newsroom/5-things-about-cms-finalized-policies-for-2019
- (20)http://www.medpac.gov/docs/default-source/reports/jun18_medpacreporttocongress_sec.pdf?sfvrsn=0
- (21)https://www2.deloitte.com/us/en/pages/life-sciences-and-health-care/articles/value-based-care-inmedicare- advantage.html
- (22)https://www.cms.gov/Medicare-Medicaid-Coordination/Medicare-and-Medicaid-Coordination/Medicare- Medicaid-Coordination-Office/index.html
- (23)https://www.cms.gov/Medicare-Medicaid-Coordination/Medicare-and-Medicaid-Coordination/Medicare- Medicaid-Coordination-Office/FinancialAlignmentInitiative/Downloads/FAExtensionMemo011917.pdf
- (24)https://jamanetwork.com/
- (25)https://www.healthaffairs.org/doi/10.1377/hlthaff.25.2.491
- (26)https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1464018/?ref=driverlayer.com
- (27)https://www.cdc.gov/mmwr/preview/mmwrhtml/su6004a12.htm
- (28)https://www.cancer.org/cancer/cancer-causes/genetics/understanding-genetic-testing-for-cancer.html
