Restricted Content
Please fill out the form below to access this content.
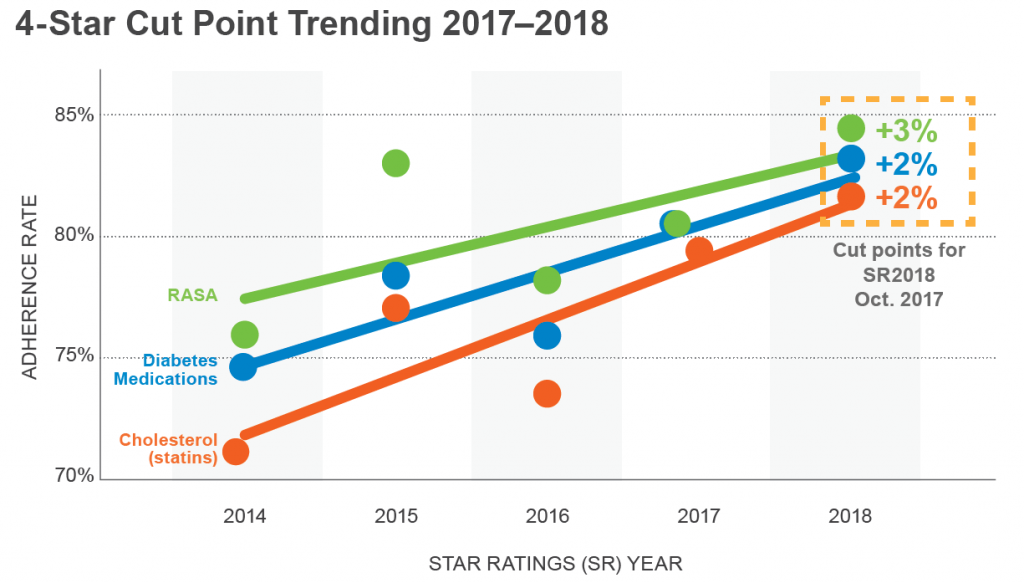
It is nearly impossible for a health plan to achieve a 4+ Stars Rating overall without high scores on the medication adherence measures, too. More than 70% of plans that achieve 4+ Stars overall also earn 4+ Stars on all three medication adherence measures. Yet, improving members’ medication adherence is a daunting task for health plans. Perhaps most challenging is that Stars’ cut points fluctuate – generally upward (see chart below) – each year based on many factors, including the aggregated performance of the managed care plans. Another challenge is that several Star Ratings’ measures assess year-over-year improvement, meaning even already high-performing health plans must push further to show adherence progress.
With the stakes so high and the bar constantly being raised, health plans look to analytics to help drive their Stars strategy. Because the best way to address non-adherence is to prevent it, predictive analytics are a key component to any winning Stars approach. The most useful analytics in this scenario inform both who is at risk of future non-adherence and also identify who is likely – through intervention – to be influenced to become adherent by the end of the Star Ratings year. Additionally, a medication adherence solution must be able to maximize the efficient use of limited resources, including by prioritizing members for intervention outreach, determining the kind of intervention that works best for each patient cohort, establishing the best time to deploy that intervention, and effectively deploying it.
Elements of a Successful Medication Adherence Strategy
Developing an effective medication adherence intervention strategy poses a number of budgetary and resource allocation challenges for health plans. Below, we identify four key questions that should be answered when designing a Star Ratings adherence strategy.
Scale – How do I best deploy my resources throughout the Star Ratings year?
In addition to understanding how many plan members must be impacted in order to reach adherence goals, health plans must understand available internal and external intervention resources compared to program requirements. If internal teams are being used for outreach, finite resources such as workforce capacity, call center volume, and training expertise must be considered. If using external resources, the plan must evaluate vendors’ solutions and capabilities, compare cost-effectiveness, and ensure the vendor has scheduling availability and capacity.
Targeting – Which members are most likely to benefit from an intervention?
Once the plan has determined which resources will be dedicated to the outreach initiatives, targeting becomes critical. It isn’t practical to contact every member in the population, and we know that a portion of the members will be adherent without any intervention and another segment will be non-adherent no matter what level of resources are directed at them. It’s those members whose adherence is urgent and still undecided that the health plan must focus on. The key is to determine: Which members can benefit from the intervention? Which members are actionable? Which members can be made adherent?
Effectiveness – What is the best way to change member behavior?
With the intervention mix chosen and the targeted population selected, the plan must next decide on the intervention mode that will be most effective for a specific member. Creating a profile for the member using key pieces of data – from complexity of their medication regimen to behavioral issues that might influence adherence – gives the plan a way to evaluate each member as to the most appropriate outreach method and actually affect member behavior.
Timing – When is the most valuable time to engage the member?
Finally, the timing of the interventions must be considered. Unlike other quality measures, where there is often a push towards the end of the year to fill gaps, medication adherence is more complex and must be evaluated throughout the year to ensure goals are met. Individual member adherence is measured by proportion of days covered (PDC) during the Star Ratings year, with a PDC rate of 80% or more considered adherent. Thus, members can appear to be adherent for the first part of the year until suddenly in September or October their status changes to non-adherent, and the plan may have missed the opportunity to intervene.
RxAnte partners with its health plan clients to address each of these adherence challenges. For instance, to determine scale, RxAnte runs simulation models – based on the health plan’s specific business rule constraints, capacity, and goals – to steer the outreach deployment plan. To target the patients with the greatest potential to make an impact, predictive analytics prioritizes members by adherence risk, receptivity to outreach efforts, and urgency of action. To impact effectiveness, health plans can leverage the integrated RxAnte contact center to perform member outreach. And to establish deployment timing, RxAnte’s predictive analytics identifies members before they become non-adherent.
Case Study: UPMC Health Plan
As one of the nation’s fastest-growing health plans and part of the top-ranked UPMC Health System, UPMC Health Plan has taken a comprehensive approach to Star Ratings. Integration of clinical data from the health system side and claims data from the insurance side gives the organization opportunities for a more broad-based approach to improving patient care and health
outcomes. For instance, UPMC uses its clinical pharmacy initiatives to steer members to participation in care and/or disease management programs.
UPMC Health Plan began working with RxAnte in 2013 and now uses a variety of services including predictive analytics, workflow solutions, and, most recently, RxAnte’s live clinical outreach program to drive continued adherence. Prior to this time, UPMC Health Plan created lists of members for adherence outreach, selecting patients who needed to refill their prescriptions and had low PDC rates. According to Jessica Daw, Senior Director of Clinical Pharmacy at UPMC Health Plan, “we knew we were missing
opportunities to affect medication adherence,” so the plan began working with RxAnte, utilizing its predictive analytics targeting strategy to deploy calls made by UPMC pharmacists—a distinctive and historically effective approach to encouraging medication adherence among plan members. “We weren’t able to devote many resources to intervention that first year, but even with just the change in the logic used to target members, we were able to see a 1 to 2 percentage point increase in our adherence rate for the 2013 Star Ratings year.”
Deployment timing was another challenge for UPMC Health Plan. “We’ve found the months of May, June, and July are often the best time to intervene,” says Daw. “Many managed care organizations try to analyze adherence data on their own, without predictive analytics. The problem is that members may appear to be adherent during the first part of the year but you don’t know
they are at risk of dropping off at the end of the year.”
Since first working with RxAnte, UPMC Health Plan has added other intervention programs, including automated refill reminders and late-to-fill interactive voice response systems (IVRs), as well as calls from pharmacy technicians and representatives which have the benefit of real-time live outreach without the expense and capacity limitations of utilizing pharmacists. It’s important
to have a diverse mix of intervention types, Daw says, in order to match the member to the appropriate outreach approach
for their specific needs while still being sensible to cost-effectiveness. The graph below depicts UPMC Health Plan’s consistent increase in adherence beginning and building their collaboration with RxAnte in 2013.
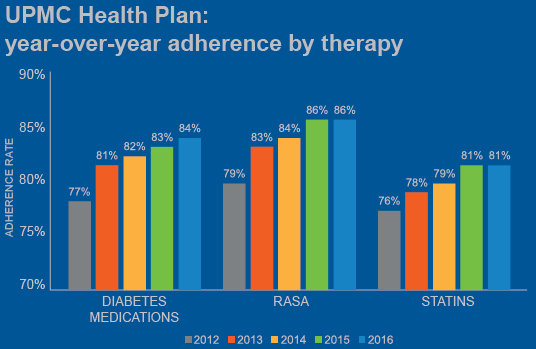
Playbook Strategy: Maximizing Value in Three Steps
UPMC Health Plan, a large regional health plan that is part of a top-ranked health system, began collaborating with RxAnte in 2013 to improve its performance among the Star Rating’s triple-weighted medication adherence measures. This collaboration entails a three-step process that has demonstrated consistent year-over-year improvement in UPMC Health Plan’s member population adherence rates.

Step 1: Set program strategy
RxAnte uses analytics across all aspects of program strategy and operations, including:
- Developing goals and setting expectations
- Prioritizing members
- Monitoring program deployment against objectives
The RxAnte Adherence Score™ quantifies individual members’ likelihood of being adherent to their drug regimen. In order to make this information actionable, RxAnte performs hundreds of iterations of expected outcomes based on various combinations of interventions.
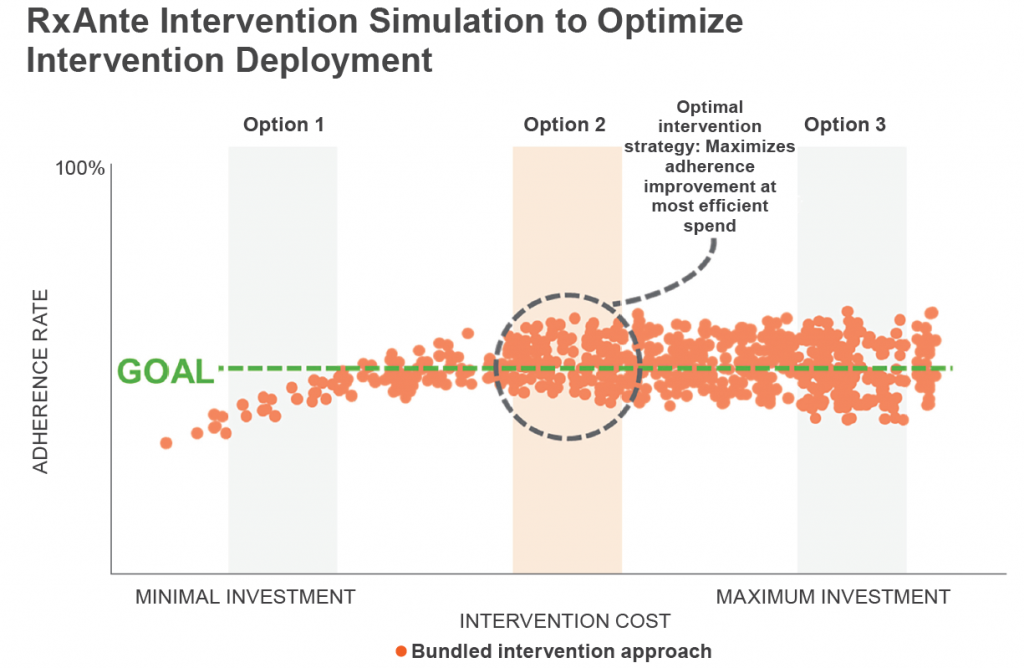
In the chart above, each of these “bundles” of interventions is represented by an orange dot. As investment in intervention activity increases, the adherence rate increases – but only up to a point. Beyond the resource spend of the Option 2 intervention strategy, adherence rate improvement flattens out and there are diminishing returns on additional outreach investment dollars.
Set achievable program goals.
By quantifying anticipated improvement and cost associated with different potential intervention scenarios, health plans can make informed decision about scale. This analysis can help executives verify whether currently budgeted resources will be sufficient to meet adherence goals, and it can also highlight opportunities to boost performance by allocating additional resources to outreach programs.
Prioritize the right patients.
Once the program goals and objectives have been set, and resources allocated to the medication adherence therapies, RxAnte uses analytics to drive member-level prioritization on a weekly or even daily basis. The highest priority patients are determined by:
- Risk: Most likely to be non-adherent
- Receptivity: Most likely to be receptive to outreach
- Urgency: Needing outreach sooner rather than later in order to mitigate risk of non-adherence
Being able to rank members in a quantifiable manner informs targeting and timing.
Monitor and Calibrate Based on Opportunity.
Finally, RxAnte monitors program deployment and status against stated objectives and measured performance, informing effectiveness. Feedback loops quickly allow the plan to make adjustments in strategy if needed, and give perspective on longer-term initiatives and opportunities.
Step 2: Engage effectively and in a timely manner
Just as RxAnte is able to use predictive analytics to determine an individual member’s medication adherence risk score and prioritization level at any given time, it is also able to help clients target the right intervention approach for the right member at the right time. Having a portfolio of intervention approaches allows the health plan to connect with the member in a way that is most relevant to their specific status. For instance, some members may require an automated call to remind them to refill their prescription; others may need a live outreach call to discuss concerns they have about side-effects of their medication. Intervention analytics utilize both demographics and scoring data, as well as therapy information to designate the appropriate intervention or series of interventions.
Clinical call centers, although the most resource-intensive intervention, are often the most effective way to drive clinical outcomes. Especially for patients experiencing more complicated barriers to adherence, live calls may be necessary to resolve these members’ issues. For instance, for a member without transportation, the pharmacy services representative may be able to set up delivery through a mail order pharmacy or a local retail pharmacy. The health plan can supplement live calls with proactive fill and late-to-fill (LTF) automated calls for additional adherence lift.
There are also digital therapeutic approaches such as text messaging and mobile adherence apps, that can be driven by information gathered from member interactions with the contact center or IVR system.
A member with an adherence barrier such as forgetfulness, for example, might be enrolled in a text messaging program reminding them to fill their medication.
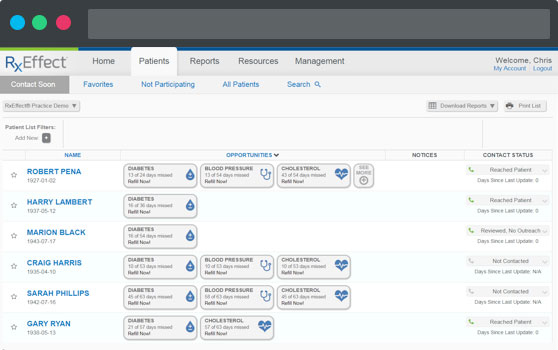
Finally, a software program can provide plans with the ability to share actionable information on members’ medication adherence and to further coordinate their outreach throughout the year. The RxEffect® workflow solution, pictured below, identifies opportunities for providers, care managers, pharmacists and others conducting face-to-face and telephone interventions with members to improve patient health outcomes. In a provider’s office, this platform gives physicians and their staff a means to use medication adherence and drug therapies as a context for addressing patients’ overall health issues. In the care management setting of a health plan, RxEffect® can act as a shared care management platform to coordinate outreach activity, offering opportunities to optimize drug therapies, share notes, and access additional resources such as motivational interviewing guides.
Step 3: Monitor and evaluate performance during and after Star Ratings year
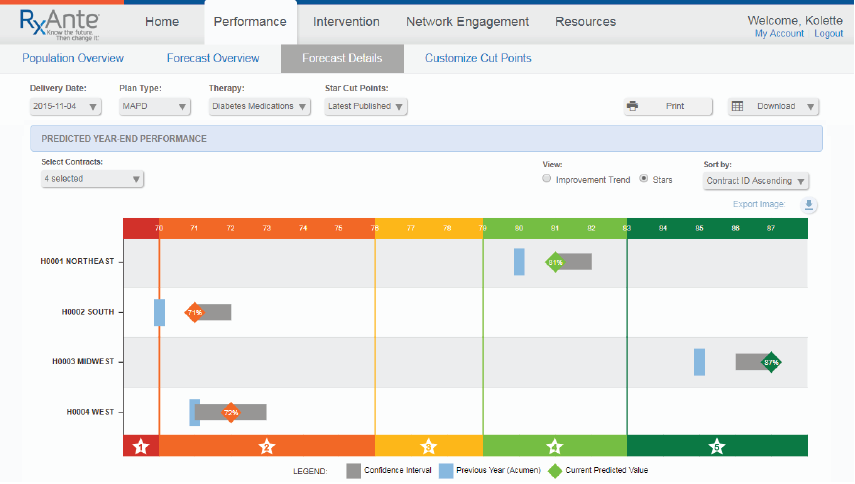
A critical part of RxAnte’s evaluation process is performance forecasting. RxAnte offers forecasting to plans at summary and contract levels to inform them of their possible Star Rating performance throughout the year. Reports are generated on a monthly basis, with estimated Star Ratings at the contract level being illustrated with a confidence interval that gradually increases throughout the year, reflecting effects of the employed strategy on intervention performance as time passes. Together, this provides an informative view of possible resource allocations over the course of a Star Ratings year.
Once program goals have been established and interventions have been launched, RxAnte delivers operational reporting for outreach efforts. Continuous monitoring of “process fidelity” – including how quickly interventions are deployed, how frequently members are reached – ensures that analytics and intervention solutions are optimized to achieve client goals. Tracking effectiveness of intervention recommendations gives the health plan immediate insight into aspects of the program that may need adjusting in order to stay on target.
Finally, it is critical to observe the effects of interventions on improving adherence on an ongoing basis. Such reviews help to facilitate more tailored intervention programs for that member population.
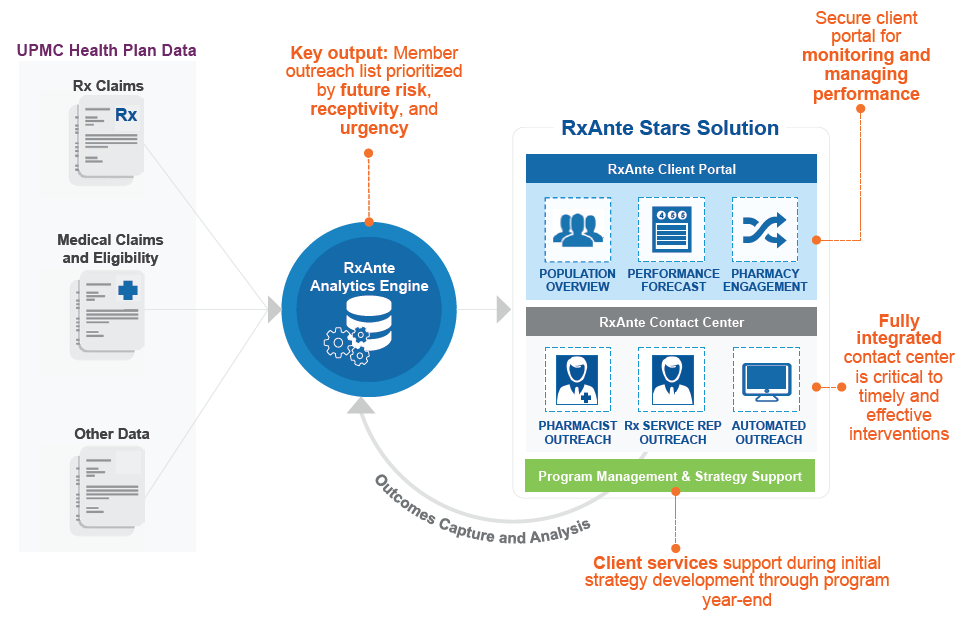
Capturing the Power of Analytics
The health plan’s pharmacy claims, medical claims and eligibility data power the RxAnte analytics engine. Other data – from results of intervention outreach to care management programs the member is participating in – are also integrated so that the analytics solution fits within the health plan’s business workflow and the context of the outreach they are performing. The plan sends information to RxAnte on a regular basis, with pharmacy claims information generally transmitted on a daily basis. The analytics solution prioritizes members by risk, receptivity and urgency, and then feeds that output back to the health plan through a client portal to: give an overview of Star Rating standings at this point, forecast performance measures to the end of the Star year, and provide key pharmacy information that can be used for additional outreach at the pharmacy or provider level.
In addition, output from the RxAnte analytics engine is integrated with the contact center and other intervention activity so that the most current information is constantly being looped back between the analytics team and the outreach team(s). A client services support department is monitoring this process to ensure all is aligned to reach improvement objectives, as well as to proactively make strategy and process improvement recommendations.
RxAnte provides formal program evaluation twice a year in order to inform plan executives of overall and intervention-level performance. A mid-year evaluation looks at results of deployments to date and whether any tactical changes are warranted for the remainder of the year. A year-end evaluation, usually presented in February following the Star Ratings year, gives insight on more long-range strategic planning and possible new initiatives.
The Future of Medication Adherence Outreach
RxAnte is partnering with health plans to find new, coordinated ways to reach members and refine member engagement protocols. To improve effectiveness of their medication adherence programs, health plans are moving toward an integrated, “surround sound” approach, with members receiving consistent messaging from different sources (health plan care management teams, providers, pharmacies, medical homes) in relevant modes (in-person, through live or automated calls, via digital therapeutics such as text messaging or mobile apps) at particular points during the year. In order for these outreach efforts to be effective, though, they have to provide the member with a solution to become adherent or maintain their adherence. Thus, the clinical, solutions-driven content of the outreach effort, along with scripting and motivational interviewing to compel the member to take action or identify and resolve barriers, are critical to success.
Beyond Star Ratings, health plans are also trying to quantify the effect of medication adherence on health care use and costs. How does improved medication adherence translate to reduced hospitalization and emergency department use? Health plans are starting to perform medication adherence outreach for asthma, COPD, and other conditions beyond those measured by the Star Ratings, as they look for ways to improve outcomes and save costs as they relate to avoidable utilization associated with chronic diseases.
